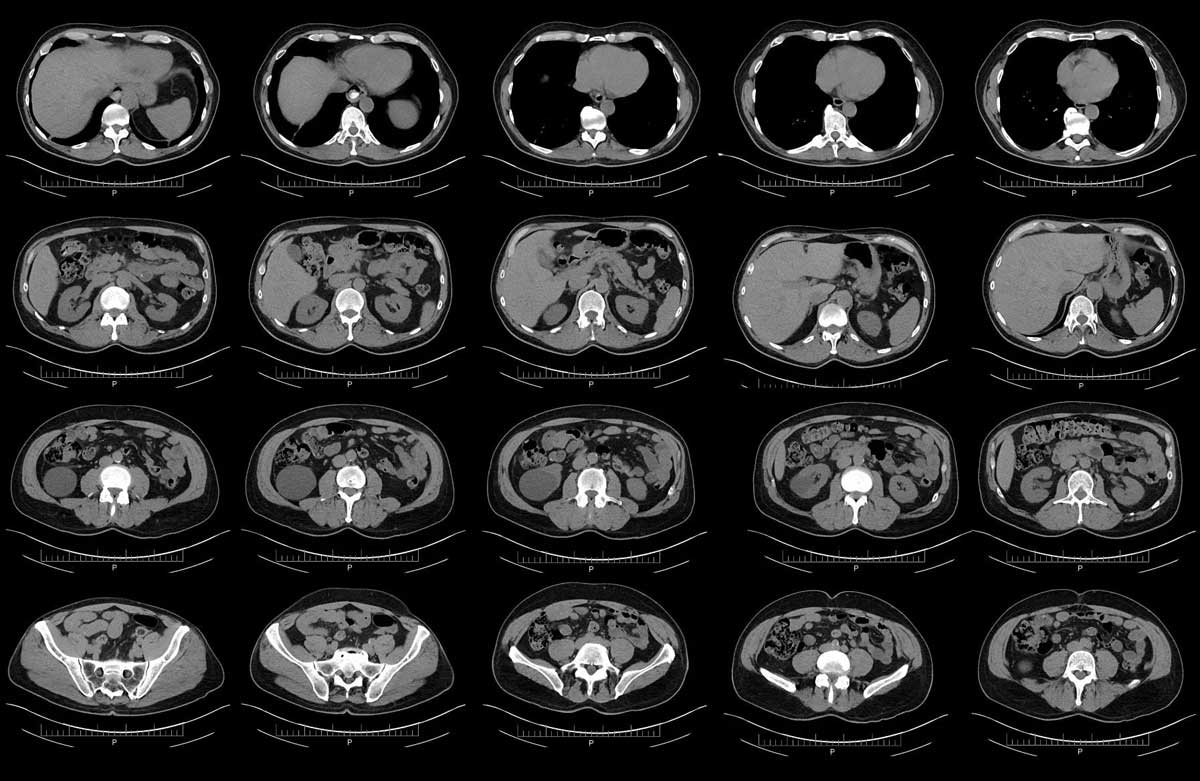
Pancreatic cancer, often lurking undetected until its late stages, has earned a grim reputation as one of the most aggressive and deadly forms of the disease. But a ray of hope emerges from the labs of MIT, where researchers have developed AI models capable of significantly improving early detection. This groundbreaking advance could change the game for millions facing this devastating illness.
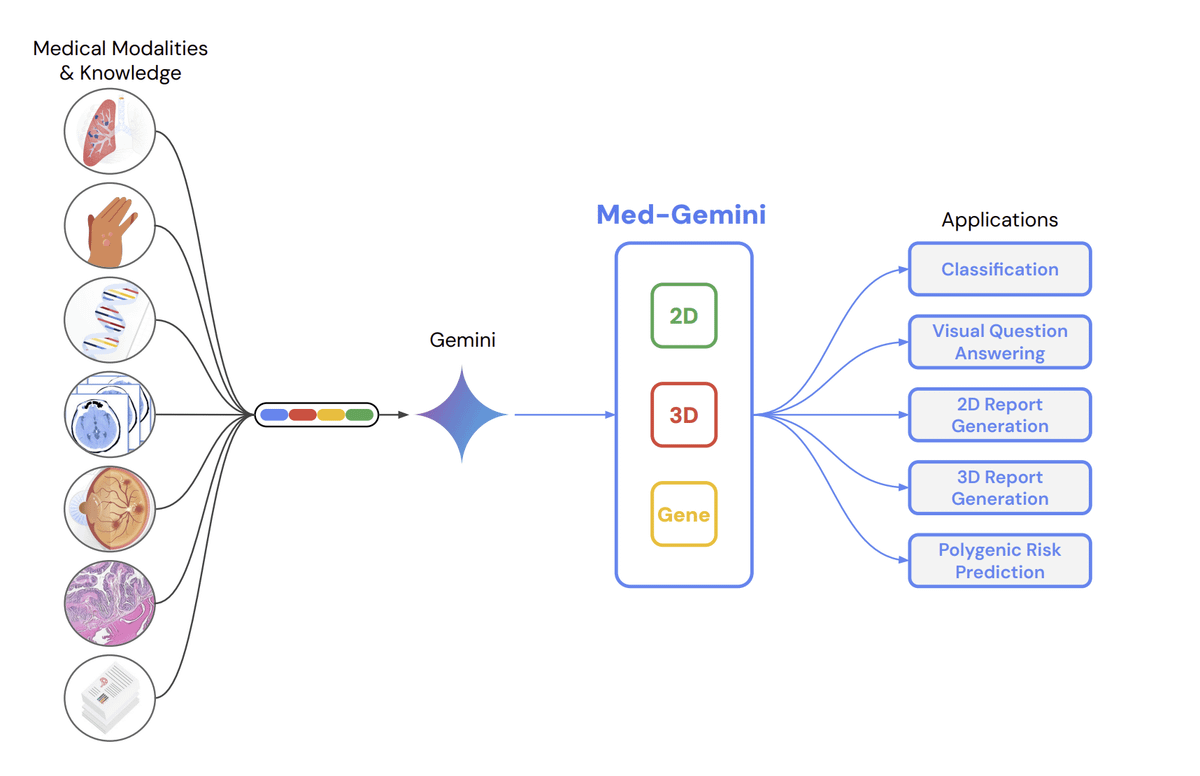
The two AI models, dubbed “PRISM,” were crafted by MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL) in collaboration with Dr. Limor Appelbaum of Beth Israel Deaconess Medical Center. PRISM works by analyzing vast amounts of electronic health record data, including demographics, medical history, medications, and lab results. By sifting through this information, the models can identify subtle patterns and flag individuals at high risk of developing pancreatic ductal adenocarcinoma (PDAC), the most common form of the disease.
“Current screening methods for PDAC are notoriously limited,” explains Dr. David Jensen, lead researcher on the project. “They often miss early-stage tumors, leading to delayed diagnoses and worse outcomes. PRISM, however, has shown remarkable accuracy in pinpointing individuals most likely to develop the disease, potentially allowing for earlier intervention and treatment.”
In clinical trials, PRISM outperformed existing diagnostic methods by a significant margin. While traditional screening methods capture only about 10% of PDAC cases, PRISM identified 35% of cases in the early stages, a three-fold improvement. This means potentially thousands more patients could be diagnosed and treated before the cancer spreads, significantly boosting their survival chances.
The implications of this breakthrough are far-reaching. Early detection is key to combating pancreatic cancer, as treatment options are far more effective when the disease is caught in its early stages. PRISM offers the potential for clinicians to prioritize high-risk patients for further testing, leading to earlier diagnoses and better long-term outcomes.
The researchers emphasize that PRISM is not intended to replace existing diagnostic methods, but rather serve as a powerful tool to complement them. “We envision a future where PRISM’s AI capabilities work alongside doctors to identify high-risk individuals, prompting further investigation and potentially life-saving early interventions,” Dr. Jensen adds.
The development of PRISM is a testament to the power of AI in revolutionizing healthcare. This breakthrough offers a glimmer of hope in the fight against pancreatic cancer, and its potential to save lives is truly inspiring. As further research and development progress, we can expect even greater strides in early detection and improved prognoses for patients facing this challenging disease.



Leave A Comment